
Contributing author:
Louise McCrink, MSc
Associate Director, Health Economics
RTI Health Solutions
Expanding HTA: integrating broader value elements to include societal effects
Health Technology Assessment (HTA) has traditionally focused on health gains and costs within the healthcare sector. This approach has long been foundational for decision-making on the adoption and reimbursement of medical technologies. However, over the past few years, there has been a growing realization that the true value of health technologies extends far beyond the walls of the healthcare sector and impacts broader societal elements. It’s no longer enough to assess the clinical benefits and the direct costs to healthcare payers; we must also capture the broader societal effects on patients, families, and the economy at large.
Capturing broader dimensions with new HTA tools
There is an emerging consensus that the full societal impact of new health technologies should be included in HTAs. Tools like the “impact inventory” from the Second Panel on Cost Effectiveness in Health and Medicine and ISPOR’s “value flower” have been developed to help guide HTA bodies in capturing these broader dimensions. These models aim to quantify not only the direct benefits to patients but also the indirect impacts, including quality of life, caregiver burden, social productivity, and even elements of hope or equity. Recently, the concept of Generalized Cost-Effectiveness Analysis (GCEA) has emerged as a method to incorporate these wider societal values into policy discussions, such as Medicare drug price negotiations.
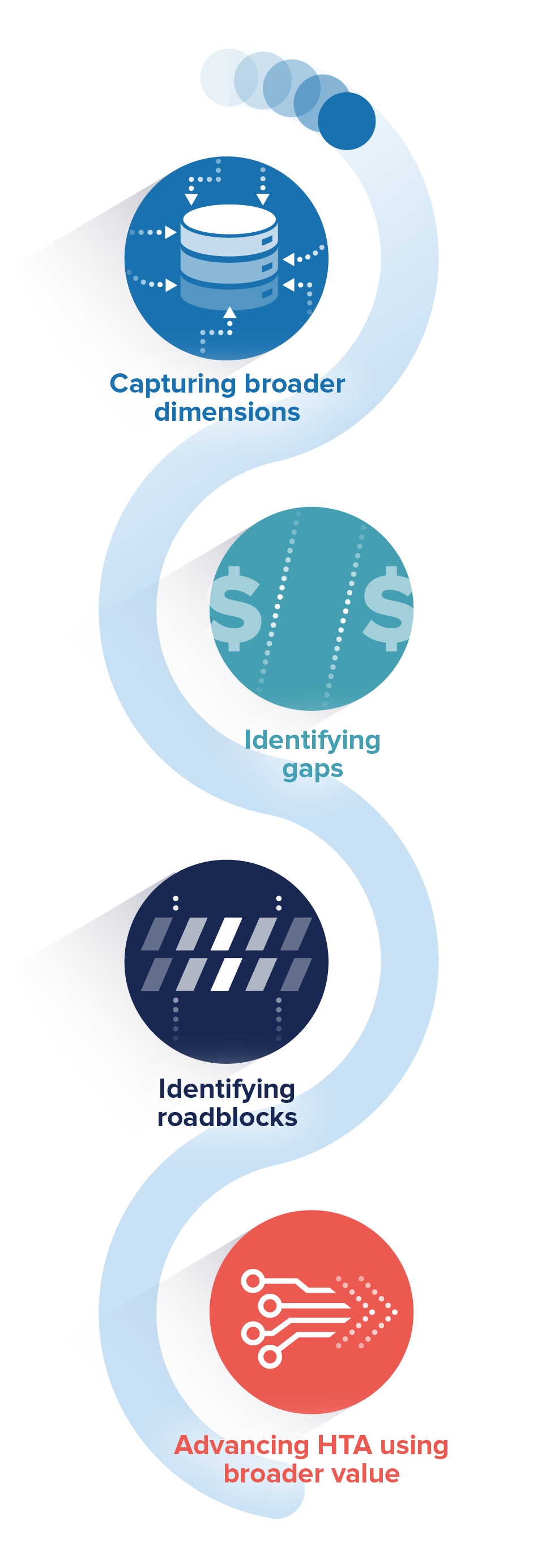 Identifying gaps in published economic evaluations
Identifying gaps in published economic evaluations
Despite these advancements, an RTI-HS methodological literature review identified a major gap: broader value elements (BVE) most likely associated with innovative drugs—such as the value of hope, family burden, equity, scientific spillover, and disease severity—are still largely absent in published economic evaluations. The review highlighted that although some BVEs, such as value of hope in oncology treatments, have been explored, they are typically not incorporated in cost-effectiveness analyses. This lack of integration can lead to an incomplete picture of the societal value that innovative drugs and health technologies provide. For instance, studies examining the potential impact of new drugs on disease severity or family burden may be excluded, skewing overall assessments.
Moreover, the review pointed to promising new analytical frameworks that could help bridge this gap. The Generalized and Risk-Adjusted Cost-Effectiveness (GRACE) model, for example, attempts to incorporate patient preferences, disease severity, insurance value, and diminishing marginal returns within value assessment. Other methods, like Distributional Cost-Effectiveness Analysis (DCEA), are designed to quantify how treatments impact health inequalities across different patient groups. While these approaches represent significant progress, HTA bodies remain cautious, with some, such as ICER (the Institute for Clinical and Economic Review), opting not to incorporate these methods yet due to challenges with implementation.
Identifying roadblocks to integrating BVEs into HTA frameworks
The roadblocks to integrating BVEs into HTA frameworks lie primarily in the complexities of quantifying these elements and the lack of consensus on how best to do so. Moreover, some question how these new inclusions would affect existing cost-effectiveness thresholds, which could shift the balance in favor of treatments that offer societal benefits but are not as cost-effective from a maximization of total population health perspective.
Even though there is a growing body of published literature on the inclusion of BVEs in HTAs, much of what is being published remains either too conceptual or too case specific. While high-level overviews provide a broad understanding of the importance of BVEs, practical guidance on their implementation remains elusive. On the other hand, case studies, though valuable, often focus on isolated instances and do not offer guidance on applying the methods to other diseases or broader policy frameworks. The uncertainty surrounding the future impact of treatments (ex-ante effects) also complicates the inclusion of some BVEs, though applying observational data from treatments that have been on the market for a few years could help build confidence in these assessments.
Advancing HTA with the inclusion of elements of broader value
Despite these challenges, there is a clear upward trajectory in the effort to quantify and incorporate BVEs into HTA processes. As more methodologies and data become available, it is likely that HTA bodies will become better equipped to address these societal impacts in the near future. The increasing number of publications and ongoing methodological developments indicate that incorporating these elements into value assessments is no longer a matter of if, but when.
Incorporating BVEs into HTA frameworks is essential to ensure that healthcare resources are allocated efficiently and that the societal benefits of new technologies are fully recognized. Not only will this promote a more efficient healthcare delivery, but it will also incentivize the development of innovations that generate the most significant benefits for society at large.
It is important for HTA bodies to be proactive in reviewing the BVEs associated with current and pipeline technologies on an ongoing basis. This continuous evaluation will help to identify the most relevant and feasible elements to prioritize and incorporate into value assessments. As methodologies evolve and data availability improves, the path to integrating BVEs into formal HTA frameworks will become clearer.
The need for further research into novel techniques and the translation of these methodologies into actionable value assessment frameworks cannot be overstated. Only then will we be able to accurately capture the true societal value of health technologies and ensure that our healthcare systems are aligned with the broader goals of societal welfare, innovation, and equity.
The time to evolve HTA frameworks is now, and by expanding our scope beyond traditional clinical outcomes and direct costs, we can ensure a more holistic, comprehensive understanding of the value that health technologies bring to society.

Additional reading:
The Inclusion of the Utility Values for Carers and Family Members in HTAs: a Case Study of Recent NICE Appraisals in the UK
Basarir H, Brockbank J, Knight C, Wolowacz S.
